From “Living Life” to Type 2 diabetes: how it really happens
Generally, people don’t just “suddenly” develop pre-diabetes. It’s not a bad week or a single takeaway that does the damage, no, it’s actually a slow drift over the years, consisting of small but significant events that all add up towards a life with Type 2.
A SLOW DRIFT : THIS IS WHAT MAKES IT HARD TO DETECT UNLESS YOU GO LOOKING!
Behind the scenes, your body is working harder and harder to keep blood sugar in the normal range… until one day the blood test says otherwise.
What follows is a general timeline of events that leads to the slow, mostly hidden decline in health and the rising prominence of Type 2 diabetes:
Year 0–3: life gets busier, movement tails off
School or uni sport ends; weekend football, rugby or hockey becomes ad-hoc; the gym bag gathers dust. Work ramps up, commuting eats time, family life needs your energy. You’re not sedentary on purpose—it just… happens.
Less muscle use means less glucose being burned day to day, so the same meals now push sugars a bit higher than they used to.
Year 1–5: convenience creeps into the diet
You still cook, but there’s more “grab-and-go”: breakfast cereals, granola, muffins; meal deals; sauces, dressings, and ready meals; Friday takeaways; more alcohol at weekends.
Hidden sugars creep in: sugary drinks and energy drinks, sweetened coffees, yoghurts, cereal bars, ketchup/BBQ sauce, and even “natural” options like fruit juice and smoothies—which count as free sugars just like table sugar and are limited in UK guidance to help protect health.
The NHS advises adults to keep free sugars to no more than 30 g per day; Bear in mind nearly a quarter of added sugars in the UK diet come from sugary drinks (a regular can of cola has ~35 g) so that’s it in one go!! (nhs.uk)
Year 2–8: “Not particularly overweight, thin even ? Don’t be fooled!!!”
You can look fine in a T-shirt and still be storing the wrong kind of fat. Visceral fat sits deep inside the abdomen around organs; liver fat (MASLD/NAFLD) accumulates inside the liver. You can’t pinch these.
They’re metabolically active and strongly linked to insulin resistance—the core problem that pushes people towards type 2 diabetes. The NHS and major clinics flag fatty liver as common and often silent; it’s tightly tied to weight, diet and activity patterns. (nhs.uk)
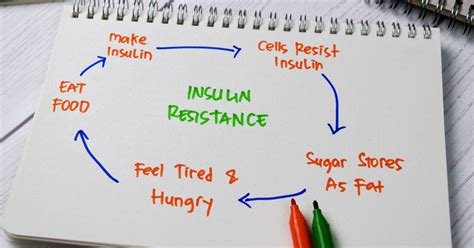
Year 4–10: the pancreas turns up the volume
As muscles and liver become less responsive to insulin, the pancreas compensates: it releases more insulin to keep blood glucose normal. This can go on quietly for many years.
Beta cells are the insulin-producing cells of the pancreas and research estimates insulin resistance and beta-cell strain precede type 2 by roughly a decade (and measurable beta-cell decline can be seen more than 10–12 years before diagnosis). Eventually, the system can’t fully compensate—fasting glucose and HbA1c start to climb into the pre-diabetes range. (NCBI).
Quick pancreas note (we’ll save the deep dive for a separate post):
When the body demands more and more insulin, those cells work overtime. Over years, output falters, especially if liver/muscle fat and inflammation persist—insulin resistance rises, insulin supply struggles.
Along the way: time-poor choices and missing knowledge
When you’re tired and pressed for time, ultra-processed foods and takeaways are easy wins. Labels are confusing; “no added sugar” doesn’t always mean low sugar (fruit concentrates still count as free sugar).
Many of us haven’t kept up with newer science—for example, how the gut microbiome interacts with metabolism and glucose control; or how sleep and stress alter appetite hormones and insulin sensitivity.
These aren’t moral failings—they’re predictable outcomes of modern life. The fix is usually small, repeatable changes, not perfection.
The blood test that finally catches it
| Test | Normal | Pre-Diabetes | Diabetes | Notes |
|---|---|---|---|---|
| Fasting Plasma Glucose (FPG) | Below 5.6 mmol/L | 5.6 – 6.9 mmol/L | ≥ 7.0 mmol/L | After fasting ≥ 8 hours |
| Hemoglobin A1c (HbA1c) | Below 5.7% | 5.7%-6.4% | >6.5% | ~3-month average |
How common is Type 2 diabetes in the UK right now?
Most people feel no symptoms—which is why the journey feels “sudden” when it’s not
- Pre-diabetes (non-diabetic hyperglycaemia):
Latest NHS England figures show 3.6 million people registered with a GP had pre-diabetic blood sugars in 2023, up 18% from 2022. The ONS estimates about 1 in 9 adults in England (≈ 5.1 million) met biochemical criteria for pre-diabetes over 2013–2019. (NHS England) - Diabetes overall and Type 2:
Diabetes UK reports over 5 million people in the UK now live with diabetes (most of these are Type 2). Official surveillance shows Type 2 prevalence recorded in adults in England reached ~7.0% by March 2024, and the charity’s latest briefing says about 1 in 5 UK adults now live with diabetes or pre-diabetes combined (≈ 12 million people). (Diabetes UK)
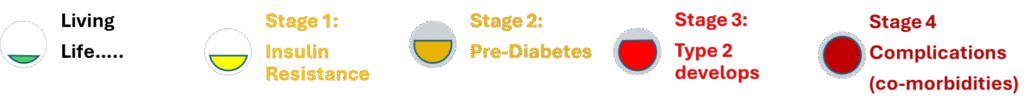
Bottom line: pre-diabetes is common, grows over years, and is driven by insulin resistance—fueled by inactivity, high free-sugar intake (including juices/smoothies), and hidden visceral/liver fat you can’t necessarily see.
Turning the tide – practical advice to tackle pre-diabetes before Type 2 can take hold
Initially, the full impact of diabetes is some way off but starts with insulin resistance. Below are some examples of actions you can take to improve your health. You will notice it’s not new advice!
- Move most days. You don’t need to recreate school-team training—brisk walking, short strength sessions, and getting back to something you enjoy (five-a-side, touch rugby, a couch-to-5k plan) make muscles soak up glucose again.
- Cut free sugars. Swap sugary drinks/juices for water or sugar-free options; watch sauces, cereals, “healthy” snacks; aim for ≤ 30 g/day free sugars. (nhs.uk)
- Protect the liver. Favour whole foods (protein + fibre + healthy fats), reduce alcohol binges, and chip away at waist size—liver fat usually improves with steady weight loss and better sleep. (nhs.uk)
- Sleep & stress count. Both can worsen insulin resistance; small improvements help the pancreas.
- Stay curious. Keep an eye on credible sources about gut microbiome and metabolic health; this field is moving fast.
If you’ve just been told you’re “borderline” or pre-diabetic, that’s not a verdict—it’s an early warning. The same long, slow path that got you here can be walked back with small, boring, consistent changes that work with your life.
📚 Sources
- NHS England update on people at risk / pre-diabetes counts (2023). (NHS England)
- ONS estimate: ~12% of adults in England with pre-diabetes (≈ 5.1 m). (Office for National Statistics)
- Diabetes UK: >5 m living with diabetes; ~1 in 5 adults with diabetes or pre-diabetes combined. (Diabetes UK)
- Type 2 prevalence in England (Public Health England/Office for Health Improvement & Disparities, March 2025 commentary). (GOV.UK)
- NHS on free sugars and fruit juice/smoothies; UK daily limits. (nhs.uk)
- NHS/Cleveland Clinic on fatty liver/visceral fat. (nhs.uk)
- Insulin resistance and long lead-in before type 2 (StatPearls; Fonseca review). (NCBI)
- American Diabetes Association (ADA) Standards of Care in Diabetes 2024
- World Health Organization (WHO) diagnostic criteria
- NHS (UK) Diabetes Prevention Programme 2024
Academic References
👀 You wanted proof — here it is!
Research clearly shows that poor diet, lack of activity, broken sleep and poor weight control are the most powerful drivers of type 2 diabetes risk. ... Read Full Article
Change Process
From Diagnosis to Direction: A Change Management Process for Type 2 Diabetes
A Type 2 diagnosis can feel final — but it’s not. What it really represents is a point somewhere ... Read Full Article
Insulin Resistance Explained
Understanding Insulin Resistance: The First Step Toward Type 2 Diabetes
Most people have heard the term “insulin resistance”, but few really understand what it means — or how quietly it can develop ... Read Full Article
So you got Pre-Diabetes
You have pre-diabetes but what does that really mean and what will you do about it?
For some, it feels underwhelming: the seriousness doesn’t quite sink in. After all, plenty of ... Read Full Article