From Diagnosis to Direction: A Change Management Process for Type 2 Diabetes
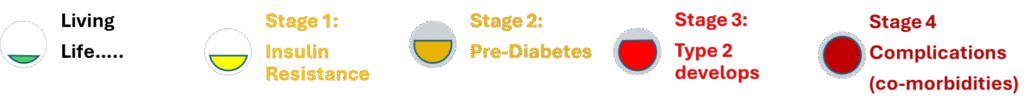
A Type 2 diagnosis can feel final — but it’s not. What it really represents is a point somewhere along a
metabolic continuum, beginning with insulin resistance and, if left unchecked, progressing through
pre-diabetes, Type 2 diabetes, and eventually serious co-morbidities such as heart disease, kidney failure, or neuropathy.
Understanding where you are on that spectrum is the starting point for change.
Like any complex system, metabolic health can be managed, corrected, and sustained through the same kind of structured approach
used in organisational change. This six-stage process provides a clear framework for moving from “current reality”
to lasting remission and renewed health.
1. Current Reality — Where Are You Now?
Every person with Type 2 is somewhere within four metabolic stages:
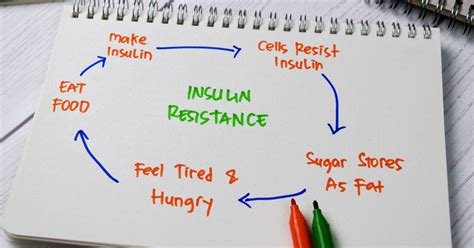
- Insulin resistance – cells are becoming less responsive, but glucose levels may still appear “normal.”
- Pre-diabetes – fasting glucose and HbA1c begin to rise.
- Diagnosed Type 2 diabetes – sustained hyperglycaemia, often requiring medication.
- Type 2 with co-morbidities – cardiovascular disease, neuropathy, fatty liver, kidney impairment, and other complications.
You are one of these stages right now. Type 2 is not benign — it can be as destructive as cancer or heart disease if unmanaged.
Yet, unlike most chronic conditions, it is also uniquely modifiable and potentially reversible through targeted lifestyle change.
2. Future Vision — Defining “Healthy Again”
What does success look like? For many, it’s normal blood sugar without medication, stable weight, healthy liver function,
and the return of consistent energy. That vision is achievable through:
- Dietary realignment — whole, unprocessed foods; reduced refined carbs.
- Fasting protocols — giving insulin a chance to fall and fat metabolism to resume.
- Regular movement — light resistance or daily activity, not necessarily intense exercise.
This is your “To Be” state — the version of you no longer defined by medication or symptoms.
3. Barriers to Success — What Will Stop You?
Change fails when internal or external barriers are ignored:
- Old habits and emotional eating
- Social pressure and unsupportive environments
- Fatigue, stress, and poor sleep
- Lack of clear guidance or tracking
Identifying these obstacles early is essential. You can’t dismantle what you haven’t named.
4. Sustainers of Success — What Will Keep You Going?
Support systems and positive reinforcers make change durable:
- Education and self-monitoring (CGM, glucose logs, fasting trackers)
- A supportive community or accountability partner
- Incremental wins — reduced glucose averages, better sleep, smaller waistline
- Mindset: treating each slip as data, not defeat
Sustainability comes from structure, not willpower.
5. What If I Do Change — and What If I Don’t?
Two possible futures exist from this point:
- If you change: blood sugar normalises, medication can often be reduced or stopped, energy and mental clarity return, and long-term risks fall dramatically.
- If you don’t: insulin resistance deepens, weight and fatigue rise, and the probability of complications — stroke, kidney disease, amputation — climbs with each year.
This comparison isn’t guilt — it’s clarity. Seeing both paths side-by-side strengthens resolve.
6. Commit to Action — Turning Intention Into Movement
All change management ends with commitment:
- Choose one action today — perhaps a 16:8 fast, removing sugary drinks, or walking after meals.
- Set a measurable short-term goal — a 7-day fasting window, a 0.5 kg weight drop, or a 0.5 mmol/L glucose improvement.
- Track, review, and iterate.
Small, consistent actions transform metabolic systems over time.
The process that rebuilds organisations can rebuild bodies too — systematically, measurably, and permanently.